Mitochondrial DNA fragment losses predict Parkinson’s disease before symptoms appear
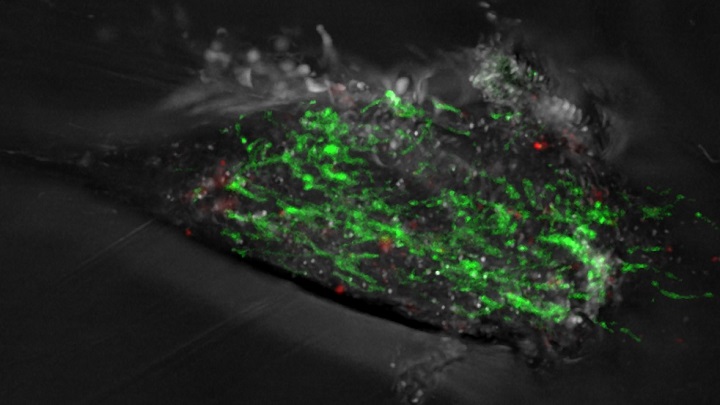
The survival of neurons, unlike most other cells in the body, depends largely on the energy provided by mitochondria, intracellular organelles that contain their DNA to function properly. The presence of mitochondrial DNA with deletions — the loss of fragments of DNA sequence — in cerebrospinal fluid could be an early marker of severe brain disease and an initial link in the whole neurodegenerative process, leading to the motor and cognitive symptoms associated with these disorders.
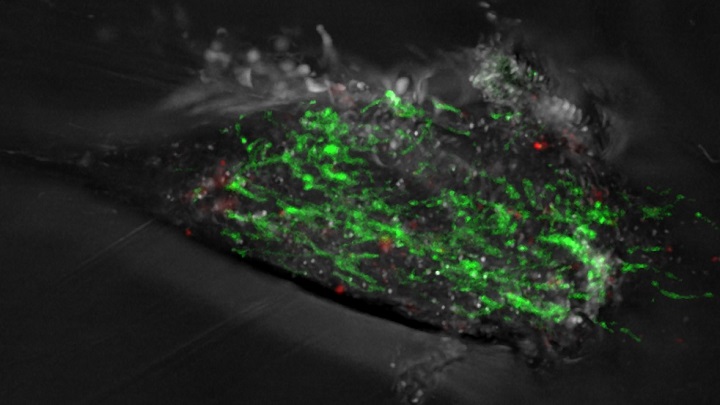
The survival of neurons, unlike most other cells in the body, depends largely on the energy provided by mitochondria, intracellular organelles that contain their DNA to function properly. The presence of mitochondrial DNA with deletions — the loss of fragments of DNA sequence — in cerebrospinal fluid could be an early marker of severe brain disease and an initial link in the whole neurodegenerative process, leading to the motor and cognitive symptoms associated with these disorders.
An alteration in the deepest sleep phase
The study was carried out thanks mainly to funding from the Michael J. Fox Foundation in the United States. As part of the study, the team studied a cohort of patients with a sleep behaviour disorder that occurs during the REM (Rapid Eye Movement) phase, known as iRBD (idiopathic rem sleep behaviour disorder). It is a disorder consisting of a disturbance of the deep sleep phase, characterised by a lack of muscle relaxation and the execution of abrupt and violent movements of the limbs and trunk, which are associated with aggressive dreams.
Over the years, many patients with iRBD go on to develop Parkinson's disease or Lewy body dementia, which is why it is thought to be an early stage of these conditions. In both cases, abnormal round protein deposits — Lewy bodies — form in the brain and are associated with neuronal death.
A previous mechanism to Parkinson’s symptoms
In collaboration with the Sleep Disorders Unit of the Hospital Clinic of Barcelona, the team analysed samples from seventy-one patients. As a result, a total of thirty-four patients diagnosed with REM sleep behaviour disorder developed Parkinson's or Lewy body dementia years later; seventeen were diagnosed with REM sleep behaviour disorder but did not suffer from any disease, while twenty formed a control group without sleep behaviour disorder or Parkinsonism.
“We have found that patients with REM sleep behaviour disorder have higher levels of mitochondrial DNA with deletions compared to the control group”, says Trullàs, CSIC research professor and leader of the molecular mechanisms of neurodegeneration group at CIBERNED.
Margalida Puigròs says that “patients with REM sleep behaviour disorder, both those who subsequently developed Parkinson's disease and those who did not, had more mitochondrial DNA circulating in the cerebrospinal fluid with deletions — that is, with losses of some fragment of genetic material — than the control group”. “However —she adds—, the most relevant finding is that we have observed that the amount of DNA with deletions is related to the time it takes for patients with sleep behaviour disorder to manifest clinical symptoms of Parkinson's disease”. This suggests that mitochondrial DNA dysfunction is a primary molecular mechanism of the pathophysiological cascade that precedes the full clinical motor and cognitive manifestation of Parkinson's disease.
Reference article:
Puigròs, M.; Calderon, A.; Martín-Ruiz, D.; Serradell, M.; Fernández, M.; Muñoz-Lopetegi, A.; Mayà, G.; Santamaria, J.; Gaig, C.; Colell, A.; Tolosa, E.; Iranzo, A.; Trullàs, R. “Mitochondrial DNA deletions in the cerebrospinal fluid of patients with idiopathic REM sleep behaviour disorder”. eBioMedicine, March 2024. Doi: 10.1016/j.ebiom.2024.105065.
